Stanford Report - July 23rd, 2009 - by Christine Blackman
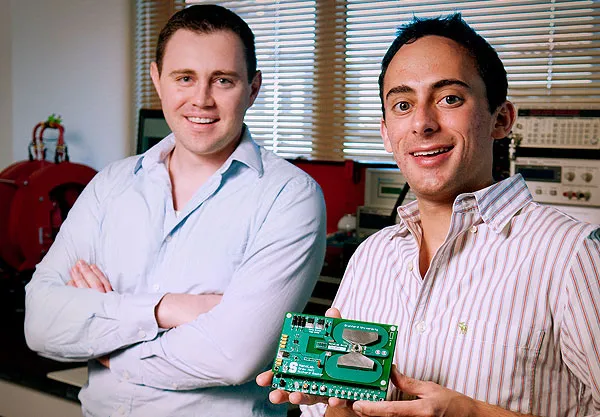
An award-winning invention by Stanford doctoral students Richard Gaster and Drew Hall may change who diagnoses diseases ranging from flu to the Human Immunodeficiency Virus. The invention, called the NanoLab, is a miniature, portable bioassay that can identify several disease proteins simultaneously without doctors, technicians or special lab equipment. With this technology, the inventors hope that individuals can literally take health care into their own hands.
“We built a technology that can be dispensed anywhere,’’ said Gaster, an MD and PhD candidate in bioengineering. “It’s affordable, easy to use, and doesn’t require a laboratory to wash anything; it’s all self-contained.”
Hall and Gaster entered a preliminary version of the NanoLab, originally coined “Lab-on-a-Stick,” in the National Collegiate Inventors and Innovators Alliance BMEidea competition as a tool to use in airports to reduce the spread of pandemics. They took first place, and at a ceremony in New York on June 10, they received a $10,000 prize and a large trophy to display in the Stanford Department of Bioengineering.
Further innovations on the NanoLab won first prize in the IEEE Presidents’ Change the World Competition as a diagnostic tool for developing countries that are short on doctors and equipment. Gaster and Hall received certificates, another $10,000, and planets named after them at a ceremony in Los Angeles on June 25.
The past, present and future presidents of the Institute of Electrical and Electronics Engineers who chose the finalists were challenged to judge diverse inventions ranging from electronic games that aid disabled children to a human-powered grain crusher.
“It was like comparing apples and oranges … but we eventually agreed that the NanoLab was No. 1,” said IEEE President John Vig. “The NanoLab is useful not only in third-world countries, and not only in poor countries, but in every country, even in the United States,” he said.
Hall and Gaster found out about the IEEE competition much later than many of their 200 competitors. They finished the project in 10 or 12 weeks while other teams of up to 20 members had worked for several months.
“It was a highly accelerated timeline,” said Hall, a doctoral candidate in electrical engineering. “We were trying to find the one sexier, killer application that would make this … something that was above and beyond,” he said. “This was something we did on the weekends, spare time and nights – squeezed in.”
The effort included planning, hard work and a bit of luck. “We planned in two cycles with basically one round worth of errors,” Gaster explained. “The first cycle failed on multiple fronts,” he said laughing. “But we figured out all the problems, and the second cycle miraculously worked.”
The NanoLab, which is the size of a small paperback book, consists of an electronic circuit board and a tiny well, just big enough to hold a few drops of blood from a pipette.
The first step is to add a droplet of a sample such as blood, saliva or urine into the well. The tester then adds magnetic tags to label the viral proteins, making them detectable by nanosensors. Each tiny magnetic sensor is similar to the read head in a computer hard drive that detects ones and zeros, Gaster said. The NanoLab uses the same technology to sense biological data. The final ingredient is a protein solution containing disease antibodies.
The tester hits start and, 10 to 15 minutes later, tiny green, orange and red light bulbs illuminate, indicating which disease proteins were detected – and at what level.
The availability of antibodies, the proteins that our immune system uses to identify and fight viruses, is the only limit to the diagnostic tool.
Part of making the NanoLab “nano” was miniaturizing a 250-pound electromagnet and a desktop computer from a normal-sized lab into tiny wires that fit in the palm of your hand. Hall built these electrical features and Gaster handled the medical technology.
“It’s a really interdisciplinary project that requires knowledge of medicine, chemistry, biology, electrical engineering and materials science,” Hall said. “I think that Rich and I complement each other pretty well. We each have different specialties and we can communicate between them,” he said.
In addition to its size and portability, the novelty of the NanoLab is its quantitative multiplex protein detection, which means it can find the level of several different diseases in one run. Diagnostic tools in developing countries typically work like a positive or negative pregnancy test – they can look at only one protein, Gaster explained. With the NanoLab, “we can look at more proteins, and we can look at them at lower concentrations,” he said.
And running the NanoLab needs no lengthy training. The students proved this by recruiting the head of their lab, Professor Shan Wang.
“We gave it to him and said, ‘Follow these instructions and see if you can detect the protein that we spiked in.’ It was his first time running an experiment in 15 years and it worked perfectly,” Gaster said.
Because the tool is portable and doesn’t require skilled technicians to run, it has the potential to sell over the counter as a home diagnostic kit. The students plan to use their prize funds for such commercial developments.
