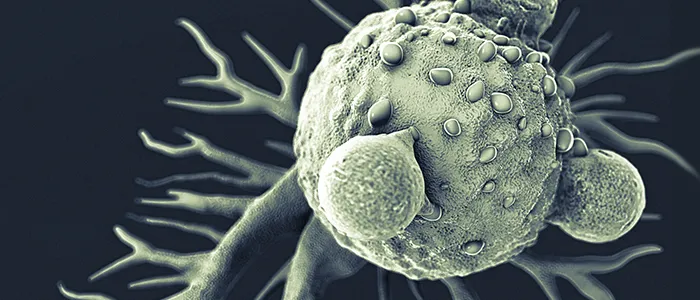
Graphic by iStock/luismmolina: T lymphocytes and cancer cell.
Stanford Engineering - March 18th, 2016 - by Krista Conger
The crew of the Proteus has one desperate chance to save a man’s life. Shrunk to the size of a large bacterium, the submarine contains a team of scientists and physicians racing to destroy a blood clot in the brain of a Very Important Person. The group journeys through the body, evading giant white blood cells and tiny antibodies while traveling through the heart, the inner ear and the brain to reach and destroy the blockage.
Although events in the film Fantastic Voyage were far-fetched when it was released in 1966, they’re now being realized every day in labs around the world, particularly in cancer treatment. A growing field called nanotechnology is allowing researchers to manipulate molecules and structures much smaller than a single cell to enhance our ability to see, monitor and destroy cancer cells in the body.
Tens of thousands of patients have already received chemotherapy drugs delivered by nanoparticles called liposomes, and dozens of other approaches are currently in clinical trials. Within the next five to 10 years, our bodies’ biggest defenders may be tinier than we could have ever imagined.
“Nanotechnology offers an exquisite sensitivity and precision that is difficult to match with any other technology,” says Sam Gambhir, professor and chair of radiology at the Stanford School of Medicine and (by courtesy) of bioengineering and materials science and engineering. “Within the next decade, nanomedicine will change the path of cancer diagnosis and treatment in this country.”
The field has some big backers: The National Cancer Institute now spends about $150 million each year on nanotechnology research and training to combat the disease; other institutes and centers at the National Institutes of Health spend an additional $300 million on nanotechnology research for cancer and other disorders. And a national alliance created by the NCI in 2004 to bring together researchers from biology to computer science to chemistry to engineering is now bearing fruit — in the form of dozens of clinical trials — at campuses and companies across the country, including Stanford.
“We can now detect just a few cancer-associated molecules or circulating tumor cells in the body in just a few milliliters of blood or saliva, or map the boundaries of a brain tumor within millimeters to assess its response to therapy or to plan a surgery,” says Gambhir. “We’ve specially designed nanoparticles that can send back a massively amplified, whopping signal when they bind to cancer cells in the colon and we’re working on ways to trigger the self-assembly of nanoparticles when they enter a cancer cell. The field has advanced tremendously in the past 10 to 15 years.”
Gambhir co-directs the NCI-funded Stanford Center for Cancer Nanotechnology and Excellence for Translational Diagnostics with Shan Wang, a professor of materials science and engineering and of electrical engineering and, by courtesy, of radiology.
The ability to diagnose the very earliest signs of trouble is crucial for efforts to stop disease in its tracks before symptoms or complications arise — which is a key component of what’s known as precision health.
As Gambhir explains, “Early diagnosis is absolutely critical, and requires an entirely different type of approach and technology than we’ve relied on in the past. Without nanomedicine, we wouldn’t have a chance of accomplishing our primary goal: to keep our hospitals empty.”
Nano schmano — what’s the big deal?
So what’s so special about nanotechnology? As you might guess, it’s a matter of scale. A nanometer is one-billionth of a meter. A human hair is about 100,000 nanometers in diameter. An average cell, about 10,000. The Proteus, on its fantastic voyage, was about 1,000 nanometers long, and the antibodies that attacked its passengers were about 10 nanometers in size.
Nanoparticles for medical use are defined as molecules or structures no larger than about 100 nanometers — comparable in size to the tens of thousands of molecules in the body that slip in and out of intact cells and wiggle harmlessly through blood vessel walls and into tissues. Like the Proteus and its crew, they can seek out and interact with individual cells and their contents. But the rules of engagement have changed, as has the possible magnitude of the visitors’ effect.
Molecules on the nanometer scale operate in a dusky netherworld where the laws of physics wobble at the edge of a quantum galaxy. Electrons behave strangely on such a tiny stage. As a result, the nanoparticles’ essential properties, including their color, melting points, fluorescence, conductivity and chemical reactivity, can vary according to their size.
Nanoscale particles also sport tremendous amounts of surface area as compared with larger particles. A cube of gold with sides 1 centimeter long has a total surface area of 6 square centimeters. But the same volume filled with gold nanospheres with diameters of 1 nanometer has a surface area greater than half a football field.
Researchers like Gambhir and his colleagues have learned how to capitalize on many of these properties in their quests to seek out and destroy cancer cells in the body, or to collect them from a blood sample for further study. By changing the size of the particles, the scientists can “tune” the nanoparticles to behave in specific ways — fluorescing varying colors for imaging purposes, for example, or grabbing onto and then releasing cancer cells for study. Some can be engineered to absorb light energy to power tiny acoustic vibrations that signal the presence of a tumor or to release heat to kill the cells from inside.
Researchers also capitalize on the particles’ vast surface area, coating them with antibodies or proteins that home to cancer cells or with signaling molecules that are released by the tens of thousands when a cancer cell is located.
Gambhir believes nanotechnology will be particularly helpful in early diagnosis and treatment. “It’s not that our therapies are poor, it’s that we apply them too late,” he says. “Nanotechnology has the potential to detect and even kill early cancer cells present in the hundreds or thousands versus the billions already present in currently diagnosable tumors.”
He and his colleagues envision a day in the not-too-distant future when nanosensors implanted in our bodies, or even in household appliances like the toilet, can alert us to the first signs of trouble — often without our conscious participation. He compares the approach to that of piloting a jet airplane.
“An airplane’s engine is constantly monitored, and information is sent to a global portal to diagnose problems in real time. We’re missing that in health care today.”
But maybe not for long.
‘Swallowing the doctor’
The concept of miniature medical minions isn’t new. In 1959, noted physicist Richard Feynman discussed the possibility of “swallowing the doctor” in a talk at the California Institute of Technology, and British researchers first realized the potential of liposomes for drug delivery in 1961. These spheres can be engineered to contain water-soluble drugs in their interior, while also squirreling away hydrophobic, or insoluble, drugs in their fatty membrane. Careful engineering can result in liposome-based structures that deliver multiple drugs in precise ratios and at high levels without the toxicities that can occur when delivering the medicines orally or through an IV. They accumulate naturally in tumor tissue, or can be targeted to specific cell types by the addition of antibodies or other molecules to their surface.
The technique was first approved by the U.S. Food and Drug Administration in 1995 to deliver the chemotherapy drug doxorubicin to patients with AIDS-related Kaposi’s sarcoma. There are now more than a dozen liposomally packaged drugs on the marketplace, and researchers have begun to explore ways to use other types of nanoparticles to deliver not just drugs, but also small RNA molecules to block the expression of specific genes or a payload of radioactivity to kill the cell.
“From a practical perspective, nano-based techniques aren’t the wave of the future. This is the now,” says Heather Wakelee, an associate professor of medicine at Stanford who focuses on the treatment of lung cancer patients. “And it’s changing how we treat patients in the clinic.”
In addition to devising new nanoparticles for use inside the body, the researchers are working on nanosensing technology for use outside the body to identify and characterize tumor cells present at minuscule levels in all manner of bodily fluids — tracking the course of known disease or even pinpointing its inception long before symptoms arise.
Wakelee has worked with center co-director Wang to design a kind of “magnetic sifter” that quickly sorts cancer cells from normal blood based on magnetic nanotags engineered to coat the cells’ surface. A key component of the technique is the ability to swiftly release the bound, living cells for further study. Another approach, also launched in Wang’s lab, involves a magneto-nanosensor — a silicon-based chip smaller than a dime that can detect and quantify magnetic nanotags on cancer cells or cancer-associated DNA or protein molecules based on changes in the chip’s external magnetic field.
This approach is being tested in clinical trials by MagArray, a company based in Milpitas, California, for its ability to detect multiple lung and prostate cancer biomarkers in patients’ blood. Like other nanotechnology, it is exquisitely sensitive.
“This technology can detect molecules present at levels orders of magnitude lower than the detection limit of current optical-based techniques like fluorescence microscopy or enzyme-linked immunosorbent assay,” says Wang. “It’s also possible to test a single sample for the presence of many different proteins or nucleic acids simultaneously in a technique known as multiplexing. This will be very useful not just for early diagnosis, but also to monitor an individual patient’s response to therapy.”
These techniques may allow researchers to not just count the circulating tumor cells in a patient, but also to sequence cells' genomes or assess the levels of expression of cancer-associated proteins on their surfaces. Wakelee is also working with colleagues to develop ways to capture and sequence tumor DNA that circulates freely in the blood of cancer patients.
“We’re looking for specific gene mutations that could change therapy,” she explains. “In this way, we’re moving away from invasive biopsies for our patients and toward a simple blood draw to learn more about an individual’s specific cancer.”
Gambhir is working to design gold and silica nanoparticles for use inside the body to detect colon cancer. The particles, which would be swallowed as pills, coat pockets of tumor cells that would normally be invisible during a colonoscopy, and can be visualized with a special endoscope designed by the team. The technique is under review by the FDA.
“These nanoparticles give highly amplified signals that just light up the bowel when bound to cancer cells,” says Gambhir.
How to monitor invisible particles
Regulatory challenges exist, of course, particularly for techniques that deliver nanoparticles directly into the body. The very ability of nanoparticles to slip into tissues and cells raises the specter of danger, particularly if the particles could become airborne or accidentally introduced into people other than the patient. The FDA and the National Institute of Environmental Health and Safety are exploring ways to ensure safety.
A critical component of nanomedicine, of course, is the ability to get the engineered particles to their destination. Although they can be targeted to a tumor via cancer-protein-specific antibodies on their surface, many of today’s studies capitalize on the fact that the blood vessels that feed a rapidly growing tumor are often leaky. As a result, nanoparticles of all stripes naturally seep out of the blood vessels and accumulate in tumor tissue.
“The FDA doesn’t yet have a clear approval process for nanoparticles intended for use inside the body,” says Gambhir. “One problem is that nanoparticles are never all exactly the same size. The manufacturing process delivers particles that might be 80 or 94 or 100 nanometers in size. This and other sources of heterogeneity means that it’s harder to get the approval from the FDA, which values homogeneity.”
Jianghong Rao, an associate professor of radiology at Stanford, is trying another approach that might be more palatable to the FDA: nanoparticles that self-assemble after they are introduced into the body as small molecules. The assembly process is triggered by the presence within a cell of a protein involved in a cancer-associated cellular death pathway. The small molecules that act as starting material for this approach are uniform in size and composition and might be more easily approved by the FDA, the researchers believe.
Gambhir compares the FDA’s current struggle to the challenges it experienced when PET imaging was on the rise in the mid-1990s. Although the agency was at first concerned about the long-term effects of the radioactive tracers injected into patients, it now has an entire arm dedicated to assessing and approving new PET reagents, which can now happen relatively quickly.
The need for new cancer treatments and the urgency for early diagnosis of particularly lethal forms, coupled with the national effort to advance nanotechnology to treat the disease, will likely mean that cancer care will soon look very different. But, as in the quest of the Proteus’ diverse crew, progress will take a concerted effort from several disciplines.
“Cancer is a very difficult disease to treat, and it’s also difficult to diagnose early,” says Piotr Grodzinski, who directs the NCI’s nanotechnology for cancer programs. “The alliance was created to bring together engineers and materials scientists, for example, with biologists and oncologists to understand, first, how nanoparticles interact with biological systems and, second, how they interact with cancer cells and what they can do to the tumor.”
“Stanford, in the heart of Silicon Valley, is a unique place for this kind of technology to develop,” says Gambhir. “The collaborative atmosphere brings together people to solve specific problems in cancer diagnosis and detection.”
The crew on the Proteus managed to band together to save the Very Important Person — in the nick of time, of course — escaping through a tear duct after destroying the blood clot in his brain just before ballooning back to normal size. Nanomedicine for future patients will likely be less fraught with urgency, but the outcome will be more important. After all, the next VIP could be you.


