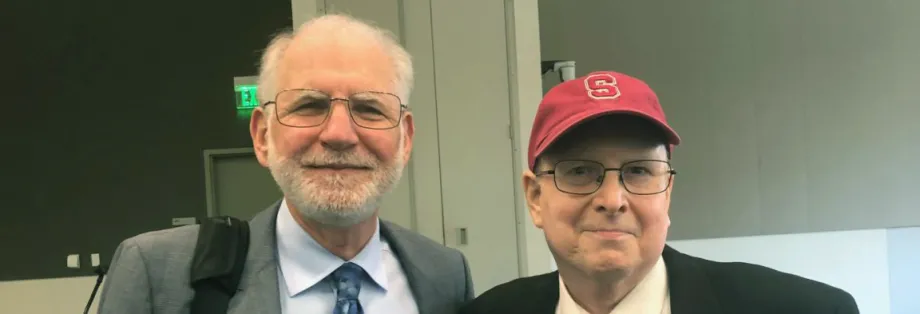
Photo by Amy Jeter Hansen: Robert Negrin (left) and David Occhipinti.
Stanford Medicine Scope - April 11th, 2018 - by Amy Jeter Hansen
David Occhipinti, then 33, had persistent flu-like symptoms, but it eventually became clear that he suffered from something more serious: acute lymphoblastic leukemia.
He underwent chemotherapy and achieved remission, but his doctors told him the cancer would return. One of them, the late Karl Blume, MD, said a bone marrow transplant might keep the cancer at bay. Occhipinti said yes, and in 1987, he became the first patient to receive such a transplant at Stanford.
“He probably was wondering, ‘Do these people know what they’re doing?’,” Robert Negrin, MD, current chief of the division of blood and marrow transplantation, said at a recent Department of Medicine Grand Rounds. “And I’m confident to say that, fortunately, because of Karl, we did know what we were doing.”
Blume had previously started a bone marrow transplantation program at the City of Hope, in Southern California, and had brought that experience to Stanford. Occhipinti's procedure signaled the beginning of Stanford’s blood and bone marrow program, which has provided transplants to more than 6,500 patients over three decades, according to program statistics.
Bone marrow transplants infuse healthy blood-forming cells into the bloodstream of people with marrow that is damaged from infection, chemotherapy or diseases, such as lymphoma, leukemia, and other forms of cancer. The donor cells travel to the bone marrow, grow and form healthy blood cells.
In his talk, Negrin outlined the program’s history in the evolving field and touched on significant research by scientists from Stanford and other institutions. He also honored Blume, for whom a lectureship was established following his death in 2013.
“Karl… was a towering figure, both physically and also with respect to his presence,” Negrin said, adding that he made the title of the speech ‘What Would Karl Do?’ “because that’s a question that we often ask ourselves.”
The first successful bone marrow transplant between identical twins took place in the late 1950s in Cooperstown, New York; however, Negrin said, the field still faced significant challenges as Stanford began its program in the late 1980s.
At that time, a donor could only be a sibling of the patient with certain matching genes. Because the immune system must be suppressed before the transplant to keep the body from rejecting the donated cells, patients were vulnerable to infections. And because the overall process — which included chemotherapy and possibly radiation — was so hard on the body, only patients 50 or younger were considered, even though older people were more likely to have diseases best treated with a transplant, Negrin siad.
Various advances have helped doctors and patients better address those obstacles over the years, he said. Now, a donor’s genes no longer need to fully match the recipient’s: a transplant can be performed if half of the relevant genes are a match. Also, scientists have discovered that stem cells from umbilical cord blood can be used in a transplant. And today a bone marrow registry, with millions of participants, increases the chance that a patient will find a match.
“In yesteryear, we would often lose patients looking for a donor, a tragedy that was really hard,” Negrin said. “These days we hardly ever lose a patient looking for a donor.”
Transplants are also more common now for older patients and those with frailer health — who are the majority of transplant patients — thanks to better matching, supportive care and control of infections, among other developments, he said. A major advancement, informed by the work of Stanford researchers and others, showed that lower-dose chemotherapy or radiation treatments before transplantation to suppress the immune system can be effective for sicker patients. “That’s a critically important advance,” Negrin said, “because [less healthy is] where our patients actually are.”
A limitation of bone marrow transplantation continues to be graft-versus-host disease, which occurs when donor immune cells see the recipient’s healthy tissues as foreign and attack them, he said. He said that he and other Stanford researchers have made progress toward understanding this potentially-fatal disease and developing effective ways to control it.
“That was another core principle that Karl brought to us, that when we have an idea that is worthy from the laboratory, to try to bring it to the patients,” Negrin said.
Negrin, who worked closely with Blume for more than 25 years, said a manuscript with instructions for the next generation of blood and marrow transplant physicians was found in Blume’s office after his death. Among seven pointers, Blume advised doctors to “follow your patients forever.”
After Negrin's talk, Occhipinti, the first to receive a bone marrow transplant at Stanford, reflected on Blume and the transplant experience more than 30 years later.
“He instilled such confidence and trust,” Occhipinti said. “He was kind of like an angel from God, as far as I’m concerned.”