
Photo by Ami Bhatt: Beverly Mitchell and Karl Lorenz met with nurses at Lagos University Teaching Hospital in
Nigeria as part of an effort to improve cancer care in the country.
Stanford Medicine News Center - April 20th, 2018 - by Ruthann Richter
During a March visit to Nigeria, a group of Stanford physicians, including palliative care expert Karl Lorenz, MD, met a young woman with advanced breast cancer that had spread to her spine, leaving her partially paralyzed. Like 80 percent of cancer patients in the sub-Saharan African nation, she had been diagnosed with the disease at a very late stage. And she had waited two years before seeking treatment.
“Patients are often impoverished, so they run the other way when they are faced with cancer. The cost, the fear and other cultural factors are all wrapped up in the reasons patients seek care late and are often lost to follow-up treatment,” said Lorenz, MD, chief of the Veterans Affairs Palo Alto Health Care System-Stanford Palliative Care Program. “They may seek advice from an imam or from a pastor or the church. They might ask for prayers for healing, but they seek out nothing else. They may not be able to afford treatment, but they are hoping for the best.”
Stanford physicians are hoping to change that outlook for Nigeria’s cancer patients through an ongoing and wide-ranging collaboration with the country’s ministry of health and doctors at the nation’s two major university-affiliated hospitals. The effort is spearheaded by Ami Bhatt, MD, PhD, an assistant professor of medicine and of genetics, who is committed to addressing global inequities in cancer care.
“It’s hard to be faced with people who are very similar to you but have been born into different circumstances and thus can’t access the services that you have,” Bhatt said. “So I’ve been driven by a sense of moral and social justice. I feel everyone should have access to the things my loved ones do, and it’s in my capacity to do something about it.”
In Nigeria, “the big leap of faith was that I decided I could do something about it, which was probably a bit audacious, but little by little we have been able to bring in more people,” Bhatt added. “And what you realize is with a relatively small part of your intellectual effort and energy, you can make big changes.”
The Stanford clinicians said the collaboration is not a one-way street and that they believe there is a lot they can learn from their Nigerian counterparts.
“Part of the dialogue we had is that we have things potentially to learn from them,” said Lorenz, who is also a professor of medicine. “They’ve managed to provide care with very little resources. We sometimes provide too much care to too many people, using too many resources. They provide the best possible care they can to as many people as they can with very few resources. We need to learn from one another.”
High mortality rates
The collaboration began two years ago when Bhatt was approached by colleagues at the Clinton Health Access Initiative and the American Cancer Society who were looking for a partner in their efforts to improve drug access and cancer care in Nigeria, where cancer is prevalent and resources for diagnosis and treatment are severely limited.
“Nigeria is a really hard place to work,” Bhatt said. “It’s Africa’s most populous country, with 180 million to 190 million people. It’s the sort of challenge where if you can solve problems in Nigeria, you can solve problems anywhere.”
Contrary to popular thinking, infectious disease is not the dominant killer in the developing world: Cancer is responsible for more deaths in low- and middle-income countries than AIDS, tuberculosis and malaria combined, Bhatt said. In Nigeria, there were more than 100,000 reported cancer cases and 72,000 deaths in 2012, with breast and cervical cancer accounting for about half of all the cancer patients, according to Globocan, a World Health Organization database. Mortality rates are extremely high, with half of all women with breast cancer dying from the disease — triple the rate in the United States.
“With people living longer from infectious diseases, cancer is becoming very prevalent, with more young women getting breast and cervical cancer,” said Beverly Mitchell, MD, the George E. Becker Professor in Medicine and Laurie Kraus Lacob Director of the Stanford Cancer Institute, who was part of the team that visited Nigeria in March. “Those are both cancers that can be prevented or detected early and can be treated effectively. So it’s a place where you can really make a difference in a country.”
Identifying pressing needs
The partnership with Nigeria began in earnest in February 2017, when a team of Stanford clinicians — including Bhatt; Shruti Sheth, MD, clinical assistant professor of oncology; Lynn Million, MD, clinical associate professor of radiation oncology; Chika Nwachukwu, MD, PhD, a resident in radiation oncology; and oncology nurse practitioner, Hope Qamoos, CNP — visited the country to talk with health care providers there about their most pressing needs. The team identified key areas where they thought they could have an impact, including improved diagnosis and drug delivery and better coordination of care between specialists.
On that visit, the team learned that the country has only nine radiation-therapy machines, and at any given time, the machines may all be broken, possibly for months at a time, Sheth said. There are also no medical oncologists nationwide and a shortage of radiation oncologists — only 30 work in the entire country — as well as a lack of patient education, limited access to effective cancer drugs and no well-defined national plan to control the disease or national registry to track trends about who has cancer and where they live.
The following summer, the same group returned with the goal of implementing changes. Qamoos began training the Nigerian nurses in chemotherapy delivery and safety. Nwachukwu developed training materials to help modernize their approach to radiation treatment planning. Million led efforts to build a cancer tumor board to facilitate care-team collaboration.
In March 2018, Bhatt and Sheth returned with a team that included Mitchell, Lorenz and Allison Kurian, MD, associate professor of medicine and a specialist in breast cancer genetics. The Stanford clinicians said that even though the health care providers they met in Nigeria are well-trained, compassionate and committed to their patients, their work has been hampered by the lack of essential infrastructure to effectively diagnose and treat the disease.
The Stanford clinicians’ first visit in 2017 happened at a time when Nigeria was developing a national cancer-control plan, and they began participating in the initiative, with Stanford researchers becoming co-authors of the plan. The plan envisions the creation of eight regional comprehensive cancer centers, and Mitchell, who led the effort to have the Stanford Cancer Center designated a comprehensive cancer center by the National Cancer Institute, is now providing guidance to both government officials and hospital leaders.
Low-cost cancer detection
On the diagnostic side, the team initially focused on breast cancer because it is so common, yet clinicians lack the tools to test for the disease, particularly among women who might have genetic mutations. “They have a lot of patients with strong family histories of breast cancer but don’t have a method for testing and prevention,” Kurian said.
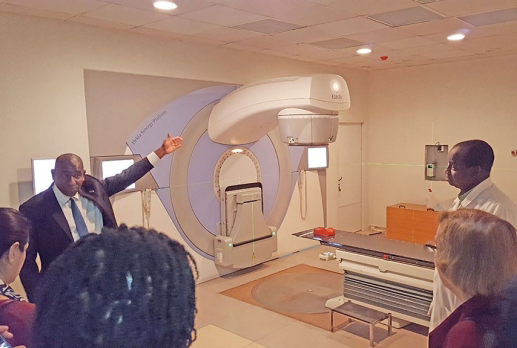
Photo by Ami Bhatt: A new linear accelerator, which is used to deliver
radiation therapy, at a hospital in Abuja.
Bhatt and Sheth arranged to have a low-cost technology for rapid breast-cancer detection shipped to the country. The system, called GeneXpert, was developed by a company in Mountain View, California. It has been used in the developing world to diagnose tuberculosis but more recently has been adapted to analyze breast tumors with estrogen and progestin receptors and to test for key breast cancer markers, such as the HER2 gene.
Bhatt and Sheth trained a group of Nigerian health care providers to use the technology and helped them launch a pilot study to test and analyze 100 samples. In March, the Stanford team learned the Nigerians had finished testing 60 samples, presenting data that Kurian said was impressive. “This may be a way to provide accurate, rapid diagnosis in a more straightforward manner and could be more broadly spread throughout the country,” Bhatt said.
The Stanford team also worked with Nigerian doctors and nurses to revamp the system for delivering chemotherapy drugs to patients. Unlike the United States, where pharmacists mix the compounds, which are then administered by nurses, the Nigerian physicians were doing both tasks themselves. Not only is the system clinically burdensome, but the physicians lacked protective equipment and were not using fume hoods to mix the medications, thus exposing themselves to potentially toxic chemicals, Sheth said.
The nurses were eager to take on the task of administering drugs to patients, so Qamoos trained six of her Nigerian counterparts on the drug-delivery methods. “They certainly felt the training was valuable as they are more aware of side effects and how to educate patients,” Sheth said.
Tumor boards and palliative care
To help improve coordination among various specialists, the Stanford team, led by Million and Nwachukwu, also helped Nigerian clinicians create multidisciplinary tumor boards, which are common in the United States. These boards involve regular meetings of specialists — for example, surgeons, pathologists, radiologists and oncologists — who discuss specific cases and then decide collectively on a course of treatment. The result is that the two major university hospitals in Nigeria now have functioning tumor boards in several cancer specialty areas.
In March, the Stanford team introduced another aspect of treatment of special interest to the Nigerians: palliative care, which is a rare specialty there, Lorenz said. Currently, Nigerian doctors and nurses volunteer their time to provide palliative care and support, at times donating a portion of their salary to help meet their patients’ needs, he said. They don’t have morphine available to help alleviate pain, but use other opioids, a less preferred option, he said.
“They provide counseling and support related to people’s questions and fears about their diagnoses and the impact on their family — the sense of shame they might feel,” he said, as cancer often carries a stigma there.
He said the Nigerian physicians were eager for more training in palliative care, requesting educational lectures that he said he would be happy to provide. He has also reached out to colleagues in the United States about possibly developing a customized training program and providing broader support for palliative care in the Nigerian medical community at large.
“Everybody is going to deal with loss, and every clinician is going to face these issues,” Lorenz said. “So it’s not an option to think about this as a job for the few. We need to cultivate a level of excellence and expertise. We want every clinician to own it.”
The collaboration is supported by a seed grant from Stanford’s Center for Innovation in Global Health, as well as funding from Global Oncology Inc., a nonprofit organization co-founded by Bhatt to create a community of people fighting cancer in the developing world.
Bhatt said she is already planning a return visit to Nigeria to continue to build on the progress they’ve made so far.
“I think what we have seen is with each visit, action is been taken by our Nigerian colleagues. It’s this nice feed-forward cycle,” she said. “We go there and suggest changes, and they not only implement them but take them one step further. It’s not only inspiring to us, but pushes you to go further. Once you realize you can make a difference, you can’t stop investing. It’s addictive.”

