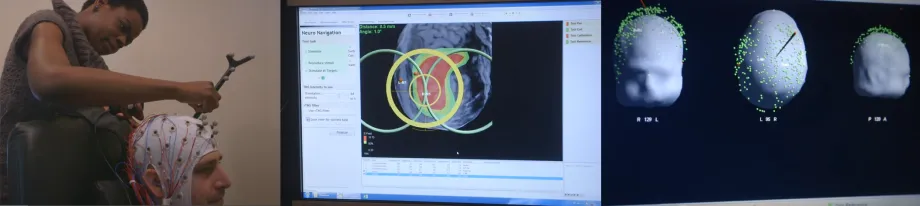
Screenshots from video by Kurt Hickman: The researchers hope to find the brain circuits that are responsible for mental health conditions, develop ways to remotely stimulate those circuits and potentially treat those conditions.
Stanford Report - November 25th, 2014 - by Amy Adams
Over the years imaging technologies have revealed a lot about what's happening in our brains, including which parts are active in people with conditions like depression, anxiety or post-traumatic stress disorder. But here's the secret Amit Etkin wants the world to know about those tantalizing images: they show the result of a brain state, not what caused it.
This is important because until we know how groups of neurons, called circuits, are causing these conditions – not just which are active later – scientists will never be able to treat them in a targeted way.
"You see things activated in brain images but you can't tell just by watching what is cause and what is effect," said Amit Etkin, an assistant professor of psychiatry and behavioral sciences. Etkin is co-leader of a new interdisciplinary initiative to understand what brain circuits underlie mental health conditions and then direct noninvasive treatments to those locations.
"Right now, if a patient with a mental illness goes to see their doctor they would likely be given a medication that goes all over the brain and body," Etkin said. "While medications can work well, they do so for only a portion of people and often only partially." Medications don't specifically act on the brain circuits critically affected in that illness or individual.
The Big Idea: treat roots of mental illness
The new initiative, called NeuroCircuit, has the goal of finding the brain circuits that are responsible for mental health conditions and then developing ways of remotely stimulating those circuits and, the team hopes, potentially treating those conditions.
The initiative is part of the Stanford Neurosciences Institute's Big Ideas, which bring together teams of researchers from across disciplines to solve major problems in neuroscience and society. Stephen Baccus, an associate professor of neurobiology who co-leads the initiative with Etkin, said that what makes NeuroCircuit a big idea is the merging of teams trying to map circuits responsible for mental health conditions and teams developing new technologies to remotely access those circuits.
"Many psychiatric disorders, especially disorders of mood, probably involve malfunction within specific brain circuits that regulate emotion and motivation, yet our current pharmaceutical treatments affect circuits all over the brain," said William Newsome, director of the Stanford Neurosciences Institute. "The ultimate goal of NeuroCircuit is more precise treatments, with minimal side effects, for specific psychiatric disorders."
"The connection between the people who develop the technology and carry out research with the clinical goal, that's what's really come out of the Big Ideas," Baccus said.
Brain control
Etkin has been working with a technology called transcranial magnetic stimulation, or TMS, to map and remotely stimulate parts of the brain. The device, which looks like a pair of doughnuts on a stick, generates a strong magnetic current that stimulates circuits near the surface of the brain.
TMS is currently used as a way of treating depression and anxiety, but Etkin said the brain regions being targeted are the ones available to TMS, not necessarily the ones most likely to treat a person's condition. They are also not personalized for the individual.
Pairing TMS with another technology that shows which brain regions are active, Etkin and his team can stimulate one part of the brain with TMS and look for a reaction elsewhere. These studies can eventually help map the relationships between brain circuits and identify the circuits that underlie mental health conditions.
In parallel, the team is working to improve TMS to make it more useful as a therapy. TMS currently only reaches the surface of the brain and is not very focused. The goal is to improve the technology so that it can reach structures deeper in the brain in a more targeted way. "Right now they are hitting the only accessible target," he said. "The parts we really want to hit for depression, anxiety or PTSD are likely deeper in the brain."
Technology of the future
In parallel with the TMS work, Baccus and a team of engineers, radiologists and physiologists have been developing a way of using ultrasound to stimulate the brain. Ultrasound is widely used to image the body, most famously for producing images of developing babies in the womb. But in recent years scientists have learned that at the right frequency and focus, ultrasound can also stimulate nerves to fire.
In his lab, Baccus has been using ultrasound to stimulate nerve cells of the retina – the light-sensing structure at the back of the eye – as part of an effort to develop a prosthetic retina. He is also teaming up with colleagues to understand how ultrasound might be triggering that stimulation. It appears to compress the nerve cells in a way that could lead to activation, but the connection is far from clear.
Other members of the team are modifying existing ultrasound technology to direct it deep within the brain at a frequency that can stimulate nerves without harming them. If the team is successful, ultrasound could be a more targeted and focused tool than TMS for remotely stimulating circuits that underlie mental health conditions.
The group has been working together for about five years, and in 2012 got funding from Bio-X NeuroVentures, which eventually gave rise to the Stanford Neurosciences Institute, to pursue this technology. Baccus said that before merging with Etkin's team they had been focusing on the technology without specific brain diseases in mind. "This merger really gives a target and a focus to the technology," he said.
Etkin and Baccus said that if they are successful, they hope to have both a better understanding of how the brain functions and new tools for treating disabling mental health conditions.



