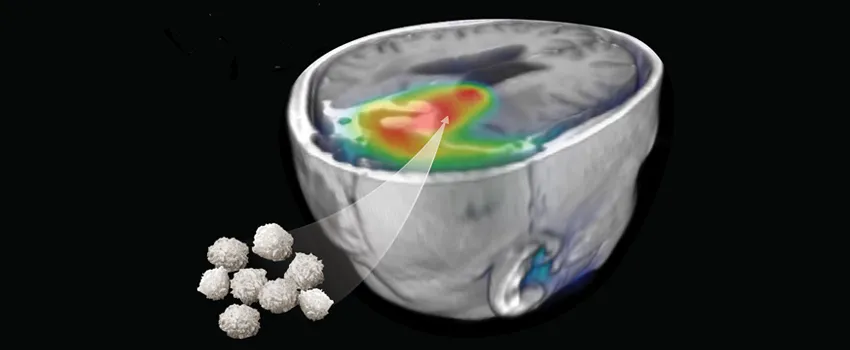
Image courtesy of J. Strommer and F. Habte: A PET scan image of the brain of a glioblastoma cancer patient shows the journey of T cells that had been engineered to attack the patient's tumor. Researchers used a technique that enabled them to track the location, numbers and viability of the introduced T cells.
Stanford Medicine News Center - January 18th, 2017 - by Jennie Dusheck
A study led by researchers at the Stanford University School of Medicine has for the first time demonstrated a way to visualize and monitor the behavior of immune cells used to treat cancer patients.
The new technique allows researchers to see where immunotherapy cells go as they hunt down tumors in the human body. The imaging technique also reveals whether the immune cells, called T cells, have found a tumor; how many T cells have arrived at the tumor; and whether the T cells are alive.
The ability to see whether T cells are attacking tumors is useful both for clinicians trying to learn if a treatment is working in an individual cancer patient and also for researchers trying to understand why immunotherapy doesn’t always work.
A paper describing the work was published online Jan. 18 in Science Translational Medicine. The senior author is Sanjiv “Sam” Gambhir, MD, PhD, professor and chair of radiology at Stanford. Lead authorship of the study is shared by former Stanford postdoctoral scholars Khun Keu, MD; Timothy Witney, PhD; and Shahriar Yaghoubi, PhD.
“We can now watch anywhere in your body where those T cells may be,” said Gambhir, who holds the Virginia and D.K. Ludwig Professorship in Cancer Research. “This is the first demonstration in humans of actually noninvasively imaging the immune system in action with reporter gene technology. It’s never been done before in a living human, and without the need to remove any tissue.”
The work was done in patients with a type of deadly brain cancer called glioblastoma, but the groundbreaking technique could be used to track immune cells targeting any kind of cancer, Gambhir said.
The limitations of immunotherapy
In one form of standard immunotherapy, a medical team harvests T cells from a cancer patient’s blood and genetically engineers them to do a better job of hunting down and killing the patient’s cancer cells. Such immunotherapy sometimes works, but most often does not. But it’s hard for clinicians to tell when it’s not working and challenging to know why it’s not.
“That’s the problem,” Gambhir said. “How do you know whether the T cells are doing their job or not? There’s no way to tell.”
Right now, the only way to find out if the T cells are attacking the cancer is to wait to see if the tumors shrink, but that can take months. And even when a treatment is working, some tumors may appear to get bigger for a while — a result of inflammation. So a temporarily enlarged tumor doesn’t necessarily mean treatment has failed. Even if clinicians are sure treatment has failed, they don’t know why. Did the T cells not reach the tumor? Or did the T cells get to the tumor but fail in their attack?
“We are shooting blind,” said Gambhir, who is also the director of the Canary Center at Stanford for Cancer Early Detection. “There are no real tools to see if treatment is working.”
It can take a medical team several months to determine if immunotherapy is working. If it hasn’t, the cancer may have spread or become more resistant, greatly increasing the likelihood the patient will die.
Releasing the hounds
Ten years ago, Gambhir and his lab began looking for ways to find out what the immune cells do once they are released back into the patient’s bloodstream to hunt down cancer cells.
The researchers first engineered T cells to better recognize the patient’s cancer cells. Later, they added a “reporter gene” to the T cells. This gene made a protein they could see with a positron emission tomography scan.
The tagged T cells are a little like bloodhounds that bay loudly as they chase down their prey. The baying tells the dogs’ human handlers where both the bloodhounds and the prey are. In the same way, the researchers could tell when T cells were near their prey — a tumor — because they could see the protein products of the reporter genes clustering there.
PET scans showing the T cells’ locations tell researchers how many T cells have reached a tumor — whether it’s 6 million cells or 50 million — and whether the cells are alive.
“And you can come back and redo the imaging after a few days, weeks or months,” said Gambhir. Repetition of the scan provides a timeline of T cell behavior.
One thing the new technique cannot do is tell researchers whether the T cells are actually attached to tumor cells. But that’s coming, Gambhir said.
“Right now, the reporter gene is always on,” he said. “But we could change the reporter gene so it only comes on after it latches onto the tumor cell and kills it.” That approach works in mice, but isn’t quite ready for human trials, he said.
Surprises
The new T cell imaging technology can also reveal, indirectly, where other unsuspected tumors are. “In one patient,” said Gambhir, “the T cells went to the tumor in the brain, as expected. But some of the T cells wandered away to another area of the brain.” Even though the second tumor had been invisible to standard imaging, the “bright” T cells in the PET scan revealed its presence.
But the biggest surprise, said Gambhir, is that the technique worked at all. “Some people are going to say, ‘This is not possible; how did they get this to work?’”
Part of it is chance and part of it is a lot of his team’s prior research efforts, he said, estimating that his lab has produced 50 papers over the last 15 years in the quest to make the T cell imaging technology work, first in animals, and, now, finally, in humans.
What T cell imaging means for patients
Glioblastoma is a particularly intractable cancer for which immunotherapies have a long way to go, said Gambhir. In all of the cases in the study, the team was able to visualize the T cells. “But in every single case, the patient still died,” Gambhir said. “So the question is, what is going wrong? Is it that the T cells just are not surviving long at the tumor site? Is the tumor too aggressive? Do the T cells kill some of the tumor cells but the rest go on?”
For glioblastoma patients, said Gambhir, the new technique will allow researchers to see immunotherapies in action and thus be better able to understand, and hopefully fix, things that go wrong with them.
The work is an example of Stanford Medicine’s focus on precision health, the goal of which is to anticipate and prevent disease in the healthy and precisely diagnose and treat disease in the ill.
Other Stanford co-authors of the paper are statistician Jarrett Rosenberg, PhD, and the Canary Center’s director of preclinical imaging core Frezghi Habte, PhD.
Researchers from the Hôpital de la Cité-de-la-Santé de Laval in Canada; University College in London; CellSight Technologies; City of Hope; University of California-Los Angeles; Sangamo BioSciences Inc.; and Seattle Children’s Research Institute also co-authored the study.
The study was funded by the National Cancer Institute (grants ICMIC P50CA114747, RO1CA082214, RO1CA135486, R01CA155769, R21NS081594 and R21CA189223); the Ben & Catherine Ivy Foundation; Sangamo Biosciences; the Wellcome Trust; and the Royal Society.
Stanford’s Department of Radiology also supported the work.
