Interdisciplinary Initiatives Program Round 12 - 2024
Project Investigators:
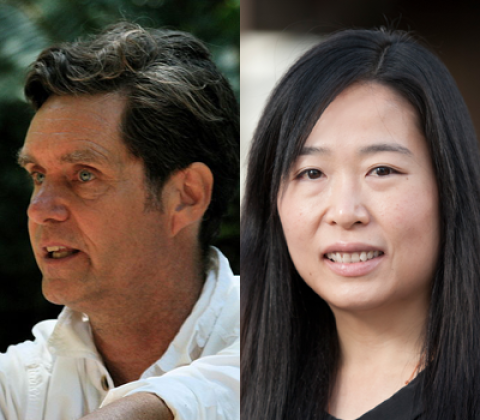
Chris Chafe, Music
Ada Poon, Electrical Engineering
Abstract:
During sedation or anesthesia, nearly all patients develop some degree of breathing obstruction. The sooner a clinician detects a respiratory obstruction, the easier it is to prevent serious adverse respiratory events. Recognizing a breathing obstruction can be challenging because a patient continues to make a respiratory effort and appears to be breathing normally, even when air flow to the lungs is completely blocked. Decades ago, anesthesiologists relied heavily on the precordial stethoscope to regularly listen for breath sounds, but the device limited clinician mobility and fell out of practice once new monitoring methods like pulse oximetry (SpO2) and exhaled CO2 (ETCO2) became available. Current monitors, however, often fail to detect these inevitable respiratory obstructions and so, clinicians rely on their senses to perform intermittent checks of breathing—like feeling with their hand for the warm breath, listening for airflow from the mouth, or watching the condensation form on a facemask. These intermittent methods are insufficient for reliably identifying, in real-time, breathing obstructions. Tracheal Acoustic Monitoring restores the useful information previously available from the precordial stethoscope. We currently have a well-functioning, wired prototype and seek to develop, via a new cross-disciplinary collaboration, a wearable, wireless version that enables real-time, AI-enabled, assessment of the quality and presence of respiratory airflow. We will conduct a clinical study to evaluate the effect of respiratory monitoring on the incidence and severity of hypoxemia in sedated/anesthetized patients. We believe that this monitor will help prevent the serious, costly, and sometimes deadly, problem of unrecognized respiratory obstruction.