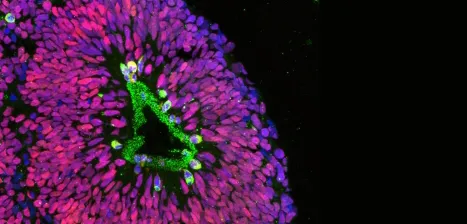
Photo courtesy of Pasca lab: A cross section of a human cortical spheroid shows divid-
ing neural progenitor cells (green) against a background of non-dividing neural cells (red).
Stanford Medicine News Center - May 25th, 2015 - by Krista Conger
The human brain is a highly organized, three-dimensional mass of cells responsible for our every move, thought and emotion. Snugly housed in the bony confines of the skull, it’s also relatively inaccessible, making it difficult to study.
Now, researchers at the Stanford University School of Medicine have devised a way to generate spherical, free-floating balls of human brain cells that mimic the architecture of the cerebral cortex, the outer layer of brain tissue responsible for how we experience and perceive the world around us and how we interact with others. The spheres contain functional neurons, working synapses and even critical support cells called astrocytes that maintain neural function. They also express genes in patterns similar to a human fetal brain midway through pregnancy.
The researchers hope that tracking the development of the cortex-like spheroids over time and observing the interactions of their cells may shed light on human brain development and the molecular causes of neuropsychiatric disorders such as autism and schizophrenia.
“One of the major problems in understanding mental disorders is that we can’t directly access the human brain,” said Sergiu Pasca, MD, assistant professor of psychiatry and behavioral sciences. “These spheroids closely resemble the three-dimensional architecture of the cortex and have gene-expression patterns that mimic those in a developing fetal brain.”
Previous attempts to create patient-specific neural tissue for study have either generated two-dimensional colonies of immature neurons that do not create functional synapses, or required an external matrix on which to grow the cells in a series of laborious and technically difficult steps.
In contrast, the researchers found they were able to easily make hundreds of what they’ve termed “human cortical spheroids” using a single human skin sample. These spheroids grow to be as large as 5 millimeters in diameter and can be maintained in the laboratory for nine months or more. They exhibit complex neural network activity and can be studied with techniques well-honed in animal models.
Pasca is the senior author of a study, published online May 25 in Nature Methods, that describes the work. Postdoctoral scholar and neonatology fellow Anca Pasca, MD, and graduate student Steven Sloan share lead authorship of the paper. (Sergiu Pasca and Anca Pasca are married.)
“The power and promise of this new method is extraordinary,” said co-author Ben Barres, PhD, professor of neurobiology, of developmental biology and of neurology and neurological sciences. “For instance, for developmental brain disorders, one could take skin cells from any patient and literally replay the development of their brain in a culture dish to figure out exactly what step of development went awry — and how it might be corrected. For Alzheimer’s disease, one could do the same to determine if the neurons or glia are abnormal and, if so, what is malfunctioning. Now we can move away from mouse as a model and instead generate functional neurons and glia from humans with literally any disease.”
Looking for a good model
The researchers embarked on the study after becoming frustrated with the lack of a good model system to study human brain development and function. Although techniques like functional magnetic resonance imaging allow scientists to broadly visualize brain activity, they don’t give an up-close-and-personal look at the complex neural networks necessary for brain function. Post-mortem tissue can give a sense of brain structure, but not of function.
“I’m a neurobiologist,” Sergiu Pasca said. “I need to study neurons that are firing.”
The researchers first created seven batches of induced pluripotent stem cells, or iPS cells, from the skin of five people. IPS cells have the ability to become nearly any tissue in the body when grown under particular conditions. They grew the iPS cells into flat, multicellular colonies on the surface of a laboratory dish. The researchers then carefully detached the intact colonies and moved them to special laboratory dishes treated to make it difficult for cells to adhere to the dishes. Within a few hours, the colonies began to fold upon themselves to create spheres. They then treated the cells with a combination of growth factors and small molecules to promote their development into neural progenitor cells. After about seven weeks, nearly 80 percent of the cells in the spheres expressed a protein made by neural tissue. Furthermore, about 7 percent of the cells expressed another protein specifically made by astrocytes — star-shaped support cells that wrap around the synapses, the junctions between neurons.
“Astrocytes are really essential to neuronal signaling,” Pasca said. “But it’s been challenging to efficiently make both neurons and astrocytes at the same time. Until now, researchers have been relying on astrocytes from rodents or human fetal tissue, and trying to grow neurons on top of them. Our system generates astrocytes that develop in concert with and are genetically identical to the surrounding neurons.”
When human cortical spheroids, or hCSs, were sliced, they exhibited architecture similar to the human cortex. “In contrast to monolayer cultures, we observed an orderly, three-dimensional arrangement of specific types of neuronal cells in the hCSs,” Pasca said.
‘Potential to bring novel insights’
That organization is primarily driven by the cells themselves, the researchers found.
“If anyone had asked me before we conducted this study what it would really take to recreate the human cortex, I would have said it would require all sorts of specific molecular cues and many other conditions of which we’re not even aware,” said Pasca. “But in reality, once the program starts, and a few conditions are met, the cells themselves are doing the rest of the job.”
The final test of the human cortical spheroids was to slice them and perform functional tests. The researchers found that up to 80 percent of the neurons in the spheres were capable of firing when stimulated. Furthermore, 86 percent of the neurons exhibited spontaneous neural signaling and participated in neural network activity.
“We’ve been treating them just like we would slices of mouse brain,” Pasca said, “and trying to answer functional questions. We’ve found that if we stimulate one side of the slice, we can record cortical activity on the other side.”
The researchers hope their study will provide a launching point for many scientists to study human brain development and function. In the long run, they hope to help patients with a wide variety of neuropsychiatric disorders.
“I am a physician by training,” Pasca said. “We are often very limited in the therapeutic options we can offer patients with mental disorders. The ability to investigate in a dish neuronal and glial function, as well as network activity, starting from patient’s own cells, has the potential to bring novel insights into psychiatric disorders and their treatment.”
Other Stanford co-authors are postdoctoral scholars Laura Clarke, PhD, Christopher Makinson, PhD, Nina Huber, PhD, and Khoa Nguyen, PhD; research assistant Jin-Young Park, PhD; senior research scientist Nancy O’Rourke, PhD; John Huguenard, PhD, professor of neurology and neurological sciences; and Stephen Smith, PhD, former professor of molecular and cellular physiology at Stanford.
The research was supported by a NARSAD Young Investigator Award, the National Institute of Mental Health (grants 1R01MH100900, 1R01MH100900, R01MH099555, T32GM007365, F30MH106261, 5R37MH060233 and 5R01MH094714), the National Institutes of Health (grants R01NS075252, R21MH099797 and R01NS092474), an MQ Fellow Award and the Korean Ministry of Science, ICT and Future Planning.
Information about Stanford’s Department of Psychiatry and Behavioral Sciences and the Stanford Center for Sleep Sciences and Medicine also supported the work.



